Though I’ve given birth to ten children, it is the delivery of my seventh baby that still haunts my memory. No novice to labor and delivery, I had learned that my body knew what to do in order to bring a baby into the world. Five had been induced, after all, and my deliveries had become quite predictable.
The labor nurse that assisted me that day apparently did not get the memo. My contractions were increasing, but I was confident it was not yet time to push, as I could feel the baby moving down. Nevertheless, the nurse instructed me to push with my next contraction.
“If you will just give me ten more minutes,” I whispered, “the baby will crown – then I will be ready to push.”
Her response stunned me. “Well, call me when the head pops out.” With that, she stormed out of the L&D room. To make matters worse, my doctor came in a short time later with a confused look on her face. “The nurse said you wouldn’t push?”
I quickly filled in my doctor (she had delivered my two previous children), but to say this nurse squashed my experience is an understatement. It was not my first, but my seventh baby, mind you, and I felt I knew enough to make the call. Although it took place over a decade ago in another state, my memory of the experience is so negative that I still get annoyed when I think about it.

Thankfully, birthing options are ever improving. “Moms are in charge of their own birth experience more and more,” says Melanie Hartman, certified nurse midwife (CNM). “The birth experience is not about the provider, but the mother,” she emphasizes. “We are just the safe-keepers of you and your baby’s health.”
Since that awful experience, I have had three more babies and I noticed each time that choices have changed. Today’s moms have a myriad of options, and most importantly, the birth of a baby has increasingly progressed to be about the mother’s desires. Approaches to pregnancy and labor are now as diverse as the babies that follow, with options in support and pain management from start to finish.
Support
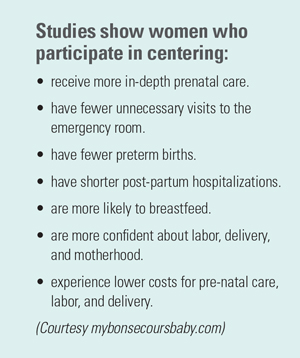
Perhaps the greatest support an expectant mom can have is someone to walk beside her through the ominous prenatal journey. The revolutionary idea of centering provides exactly that. “Centering is a national program which provides monthly group-centered prenatal care where new concepts are introduced in each session,” says Hartman, who is employed by The Woman’s Center at St. Francis Medical Center. Led by a midwife, each group consists of expectant mothers who are all due within four to six weeks of one another. Not only do the patients get to spend a 2-hour block with their provider, but first-time moms also gain insight and wisdom from the more experienced mothers in the group. What’s more, each session is relevant to current fetal development. From nutrition in the first trimester to lactation and postpartum depression at the conclusion, every aspect of caring for mom and baby is thoroughly covered.
“Supporting women with the latest methods and information is something that is very near and dear to our hearts,” says Julie Reagan, director of Bon Secours Love and Learn, which provides education and support for women from prenatal to postpartum care. Roeger says women who participate in centering not only get the education and support they need during pregnancy, but also tend to stay in touch far beyond the session’s end. “Relationships are formed and we reunite the women to share their birth stories to the group with whom they traveled that journey.”
Richmond mom of three, Meg Gomez, was excited to participate in centering throughout her third pregnancy. “The greatest thing about centering was sharing my experiences with the seven women in my group and finding that we all had similar hopes, fears, and expectations.” A sisterhood quickly developed, says Gomez, who was determined to attend her reunion despite giving birth just two days prior.
“I was discharged, went home, took a nap and headed for my reunion,” she says. “Those women were like family by the end, and I couldn’t miss meeting their babies and hearing their birth stories, as well as wanting to share my own.”
 And the bond is not easily dissolved, as social media easily enables the group to stay in touch. “We all have new babies so we may not see each other much, but we do talk about everything from lactation to car seats,” says Gomez, adding that the best thing about social media is being able to see each other’s babies as they grow.
And the bond is not easily dissolved, as social media easily enables the group to stay in touch. “We all have new babies so we may not see each other much, but we do talk about everything from lactation to car seats,” says Gomez, adding that the best thing about social media is being able to see each other’s babies as they grow.
While there is no official data, centering is strongly suspected in helping reduce postpartum depression. “The March of Dimes identified it early on as a way to help women who had the potential for poor outcomes and has found it to be very effective overall,” says Reagan. “We don’t know some of the specific numbers, but what we do know is centering forms a good support system both before and after baby arrives.”
As if prenatal support wasn’t enough, what started as a centering pregnancy group has spun off to parenting education. “Basic core classes are available thanks to the incredible array of people with whom we partner,” says Reagan. These Parenting Partners, as they are called, lead classes in everything from prenatal yoga to helping pets adjust to baby’s arrival.
“Another way we support our patients is with a family oriented experience that brings the word ‘birth’ back into the C-section,” says Hartman. The postpartum experience of what is called the gentle caesarean is very similar to vaginal birth in that both skin-to-skin contact and immediate nursing are implemented.
“Delivering a baby is not just about birth, nor is it just about the delivery by provider,” says Reagan. “The Bon Secours staff is doing a great job in providing women the experience that is desired.”
Pain Management
Undeniably, the most pressing issue on every expectant mom’s mind is pain management. One major advance in this capacity is the use of nitrous oxide. Used more commonly in Europe and only recently favored in America (and piloted by St. Mary’s, no less), nitrous oxide is administered by inhalation, the same anesthesia used during a dental procedure. “I have often seen it work for women who either don’t want or don’t have time for more anesthesia,” says Hartman. What’s more, laboring moms can enjoy the freedom of movement. “While every other option requires confinement to the bed, nitrous is very liberating in that the mom is not restricted.” Additionally, the absence of epidural or IV needles can help tame anxiety.
 For Gomez, natural childbirth seemed the ideal situation, but knowing the nitrous was available empowered her to take one contraction at a time. “I was willing to use it if necessary because I liked that it is so minimal,” she says. “With my first two, I felt that my only choices were with or without an epidural,” says Gomez, “and while nobody is trying to win an award for the most natural childbirth, it was nice knowing there was another less invasive option for relief.”
For Gomez, natural childbirth seemed the ideal situation, but knowing the nitrous was available empowered her to take one contraction at a time. “I was willing to use it if necessary because I liked that it is so minimal,” she says. “With my first two, I felt that my only choices were with or without an epidural,” says Gomez, “and while nobody is trying to win an award for the most natural childbirth, it was nice knowing there was another less invasive option for relief.”
While some stronger anesthesias make it difficult for moms to stay alert, nitrous has been a reliable resource for women who have been in transition. “Not only has the use of nitrous enabled our moms to be fully present while giving birth, but it is without the side effects of blood pressure drops or sedation of fetus and it is really safe for baby,” says Hartman. What’s more, unlike other anesthesias, the effects subside very quickly.
“We have a variety of low intervention equipment to help out,” says Reagan, who lists everything from balls to rock on to peanut balls, a large peanut-shaped pillow which is positioned between the legs to help open up the pelvic outlet. “Then there is the more technical equipment like the wireless fetal monitor which has revolutionized the ability of the laboring mom to walk around and keep moving, working with the labor by keeping baby’s head down throughout the process.” Additionally, the wireless monitoring can even be worn in the tub, which has markedly improved the experience for higher risk moms who require constant monitoring.
As another alternative to medication, a favorite of laboring moms is the labor tub. “Labor tubs are the most common forms of relief,” says Hartman, adding that while her practice does not do water births, they do have four full immersion tubs to offer water labors from advancing labor all the way to transition.
“What I appreciated about the labor tub is that I got in when it was getting really intense and I needed a breather, then I got out and got back to business,” says Gomez.
Perhaps a less familiar approach to childbirth is hypnobirthing, a method developed by Marie Mongon, hypnotherapist and author. A mom of three and physical therapist, Amy Trickett, chose the approach of hypnobirthing when another PT recommended it after Trickett had expressed a desire for an unmedicated birth.
Defined as an educational process that includes special breathing, relaxation, visualization, and meditation, hypnobirthing is all about teaching your body to relax so that it doesn’t fight against labor but instead works with it. “Hypnobirthing means practicing guided imagery while you speak to each body part and release the tension from your tissues,” says Trickett.
One tool used in this process is audio affirmations, which reinforce calmness and confidence. When Trickett’s care-giver in another state expressed concern over the baby’s size, for instance, she found that listening to the affirmations at bedtime calmed her fear by reinforcing what she already felt to be true: Her body would create the perfect size baby for her body. “It is a lot of self-talk that defeats false information and fears,” she says, adding that the affirmations also gave her the confidence to postpone a suggested induction, allowing her pregnancy to take its natural course and deliver a full-term, healthy baby.
Education is also a big part of hypnobirthing, says Trickett. “Classes provide support and positive atmosphere for both you and your birth partner,” she says, “educating both of you on exactly what is happening during each contraction so you are less afraid and can seek to understand it.”
A peaceful birth experience is another essential piece of the hypnobirthing experience. “The name was kind of off-putting to me at first, making me hesitant to try this method,” says Trickett, “but I am so glad I did because it opened up my eyes to so many options.” Keeping the delivery room quiet and dim, for instance, with no screaming or counting, created the ideal experience for Trickett. What’s more, she liked that limited procedures allowed the baby to be in control. Like centering, hypnobirthing parents reunite after their births to share each other’s stories.
No matter how it happens, the birth of a baby takes courage and tenacity. “I liken it to a marathon,” says Gomez. “I wouldn’t run a Richmond 5k without training; without getting my mind right and in the race and preparing my body.”
As the mom of ten, I would say that pretty much describes the parenting journey, too.




